Valdosta doctor provides facts on ‘flesh-eating’ disease
Published 7:00 am Saturday, June 2, 2012

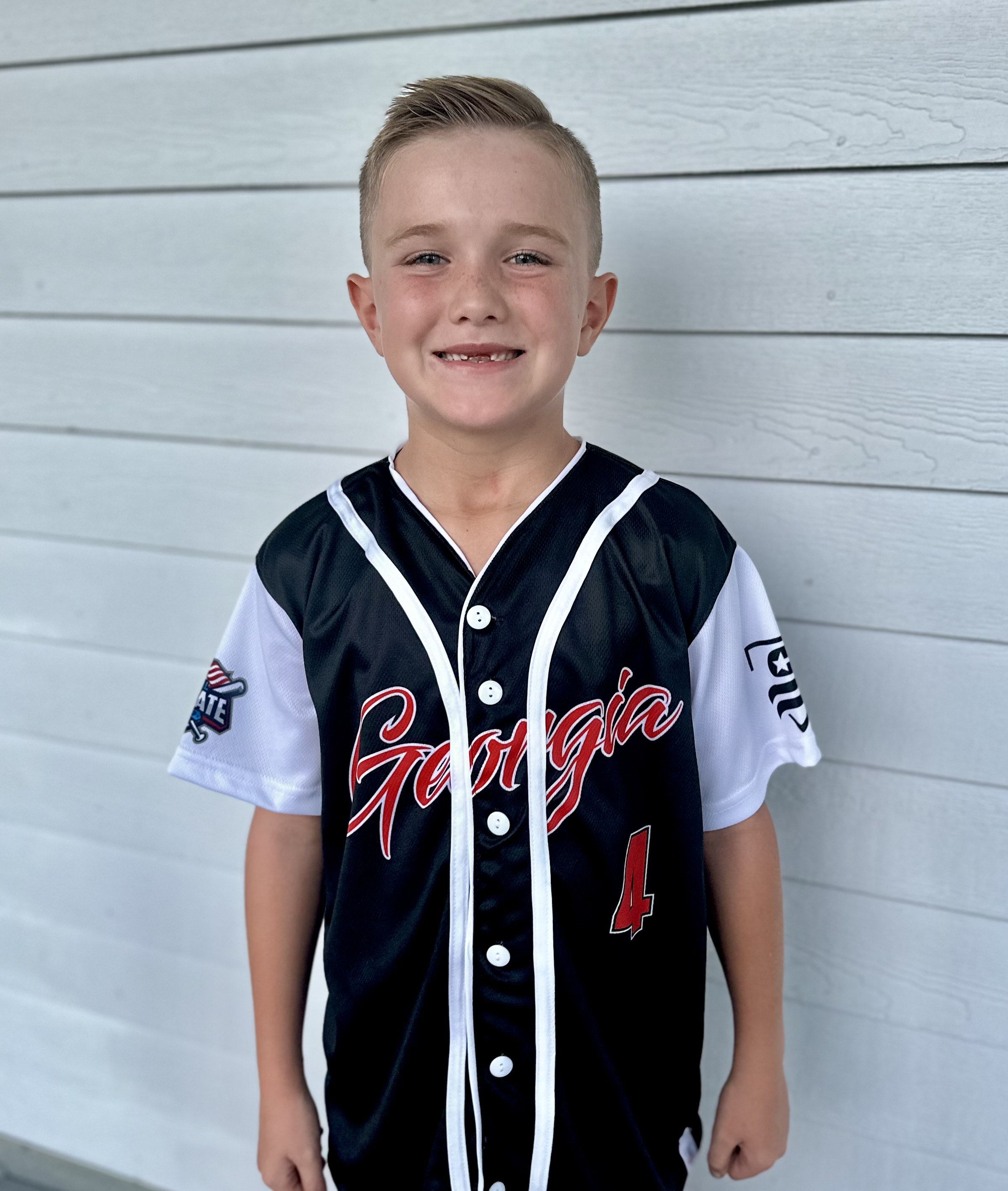
- Dr. Guillermo Saurina with one of the two hyperbaric chambers at South Georgia Medical Center. The chamber is used for a variety of illnesses, including saturating tissues with oxygen to kill bacteria causing necrotizing fasciitis.
Several serious cases recently of “flesh eating bacteria” in Georgia have garnered national publicity, and left many wondering how this serious infection can be treated and prevented.
Trending
The most publicized case is the 24-year-old University of West Georgia graduate student who went zip-lining over the Little Tallapoosa River and cut her leg, creating an opening for the bacteria to enter. According to the Associated Press, she remains in serious condition following the removal of much of her left leg, with partial amputations of her hands and right leg and foot.
With several high-profile cases so close together, the natural questions include how is the bacteria spread, are the cases related and can it happen here?
Dr. Guillermo “Willy” Saurina, an infectious disease specialist in Valdosta, shared good news and bad news about necrotizing fasciitis, the official term for the infection.
The good news is that it is not contagious (unless you rub the bacteria into an open wound), but the bad news is that it’s fairly common.
“We treat about 10 patients each year at South Georgia Medical Center with necrotizing fasciitis. It is not new. It’s been around for 100 years, but most cases are not that severe and don’t receive national attention,” said Saurina.
The infection is typically found early enough to treat it, and although partial removal of damaged tissue is not unusual, full limb amputations are not common.
Trending
Saurina said necrotizing fasciitis is simply a term for a deep muscle infection.
“Fascia is a sheet of connective tissue covering or binding together body structure, and is found around muscle tissue. When you get an infection, it typically stays close to the skin’s surface and is treated and it goes away. When the infection goes deep into the muscle, it can become necrotized (localized death of living tissue).”
Saurina said there are a number of bacteria that can cause the condition, most of which can be found on anyone.
“Many who are exposed to the bacteria may have mild symptoms, but their immune systems fight it off. In other cases, when the immune system is compromised or another disease is present, complicating symptoms, then it becomes more serious and
spreads very rapidly.”
Saurina said all the bacteria need to thrive is the right temperature,
vitamins and sugar, which they find in an open flesh wound, even a paper cut.
“It’s perfectly safe to go swimming, especially in swimming pools as chlorine kills 99 percent of all bacteria, but if you have an open sore or wound, don’t swim in pools, but especially not in rivers and lakes.”
Group A staph is the most common bacteria strain, but there are others, and it only takes the right combination of factors for the infection to become “flesh eating,” so-called because the tissue dies.
“When the infection is present and the tissue dies, you have to cut it, and you have to cut it before the area where the infection starts, so you are cutting into healthy tissue. In the case of an amputation, you can’t just cut off the infected area, you have to remove it entirely in order for the remaining tissue to survive.”
There are several ways necrotizing fasciitis is treated, beyond the removal of tissue. Antibiotics are used to prevent the spread of infection and patients are treated in a hyperbaric chamber. Saurina demonstrated the two hyperbaric chambers at SGMC, which he said are in nearly constant use to treat a variety of diseases, including cancer.
“In the case of necrotizing fasciitis, the chambers are used because 100 percent oxygen will kill anaerobic bacteria. Patients are in the chambers for up to two hours at a time over the course of several days.”
The chambers are an enclosed capsule and patients are monitored visually and by voice contact to ensure their safety. Most patients watch TV or fall asleep, said Saurina, and those who are claustrophobic can be mildly sedated if needed.
The most essential component to the infection is early detection, and Saurina said, the following symptoms are common: fever, extreme pain, redness, swelling, pus, and nausea, but one of the most telltale signs is the smell.
“Patients can give off a strong odor, like a gas smell, as the tissue begins to die.”
Saurina likened the smell to that of a decomposing body, and said the odor is an ominous sign of a severe infection.
If a physician suspects the condition, an MRI or CT Scan are used to identify the depth of the infection, Saurina said.
Only a relatively small percentage of cases are fatal, but the removal of tissue is essential, and unfortunately, can include amputation.
“It is not contagious from person to person, but you really can’t prevent it. The healthier you are and the stronger your immune system is are key factors to preventing the infection from taking hold. If it does, early detection is key to prevent the spread of the infection, but even with a case every four to six weeks or so, it is still a fairly rare disease and is not a cause for general alarm.”
For more on this story and other local news, subscribe to The Valdosta Daily Times e-Edition, or our print edition.